Severe PARDS in an Infant with a Rare FARSA Mutation Treated with Bronchoscopic Segmental Insufflation and Surfactant Therapy
Main Article Content
Abstract
Introduction: Pediatric Acute Respiratory Distress Syndrome (PARDS) is a life-threatening condition characterized by severe hypoxemic respiratory failure and lung inflammation. The pathophysiology involves surfactant inactivation and deficiency, leading to decreased lung compliance. Traditional endotracheal surfactant administration often yields inconsistent results due to inhomogeneous distribution. This case report evaluates the efficacy of bronchoscopic segmental insufflation and surfactant therapy in a patient with severe PARDS and a rare genetic mutation.
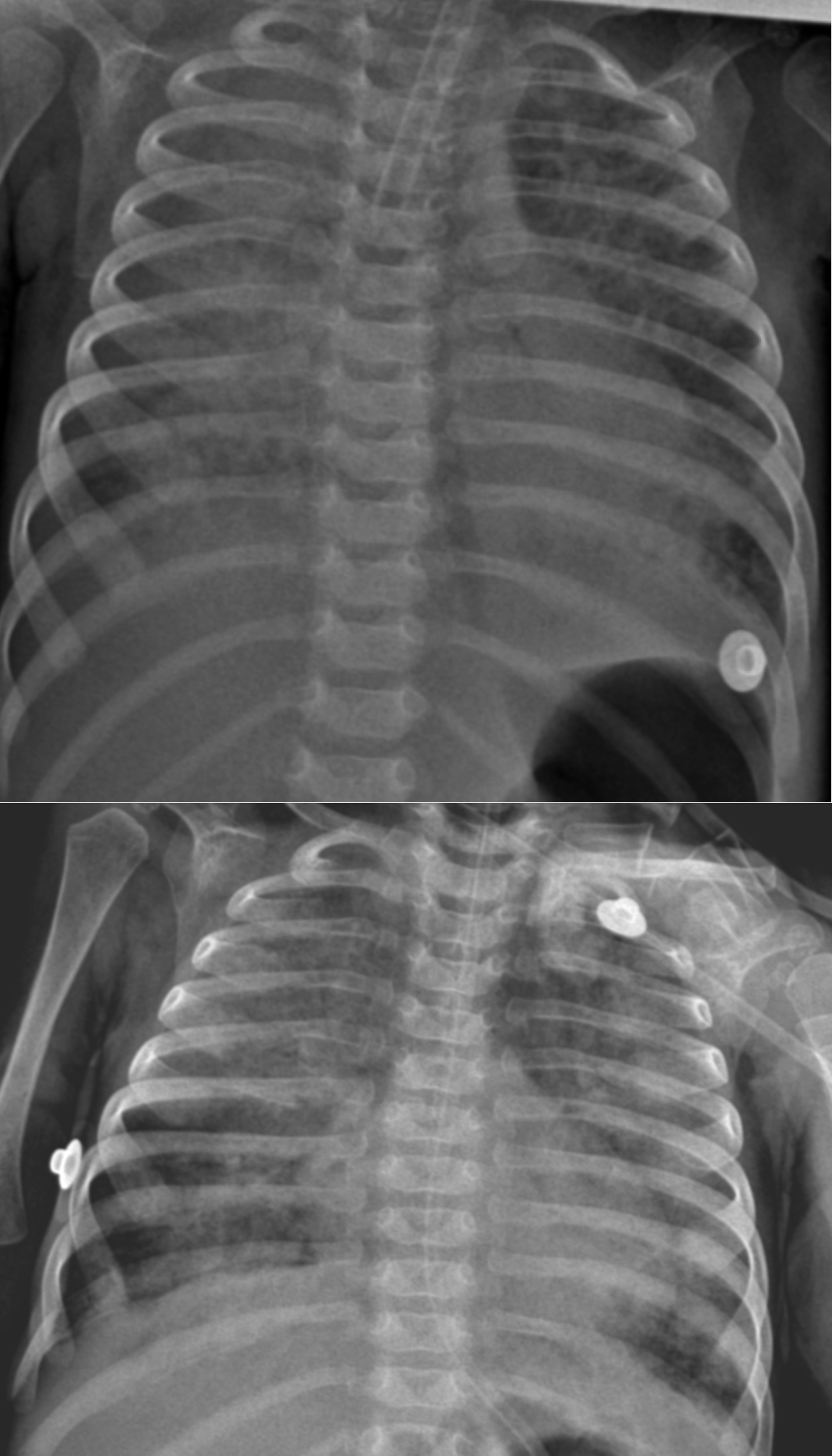
Methods: A 4-month-old female infant with severe PARDS (oxygen saturation index [OSI]: 25), growth failure, and chronic diarrhea was admitted. Due to refractory hypoxemia despite optimized ventilation (FiO₂: 100%, PIP: 35 cmH₂O, SIMV ventilation mode), a bronchoscopic intervention was performed. The procedure involved the removal of mucopurulent secretions and the administration of a total surfactant dose of 200 mg/kg (poractant alfa). The surfactant was delivered to each lobe separately using a "wedge" position, followed by pressure-controlled insufflation (30 cmH₂O for 30 seconds per segment, consisting of one initial insufflation, followed by surfactant instillation and two additional insufflation cycles) to optimize distribution.
Results: Marked clinical improvement was observed following the bronchoscopic intervention: PIP decreased from 35 to 21 cmH₂O, and OSI improved from 25 to 8. Oxygen saturation rose from 88% to 95% despite lower ventilator settings. A second identical procedure was performed two weeks later due to persistent mucus plugging and the patient was successfully extubated three days thereafter. Whole Exome Sequencing (WES) ultimately identified a homozygous c.883C>T mutation in the FARSA gene, confirming a diagnosis of Rajab interstitial lung disease.
Conclusion: Bronchoscopic segmental insufflation combined with surfactant instillation may be considered as a potential adjunctive strategy in selected cases of severe PARDS refractory to conventional management. This technique allows targeted delivery to affected lung regions, facilitates airway secretion clearance, and provides additional diagnostic utility through bronchoalveolar lavage.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Share
References
1. Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015;16(5):428–439. doi: 10.1097/PCC.0000000000000350
2. Miller AG, Curley MAQ, Destrampe C, Flori H, Khemani R, Thomas NJ, et al. A master protocol template for pediatric ARDS studies. Respir Care. 2024;69(10):1284–1293. doi: 10.4187/respcare.11839
3. Rodríguez-Moya VS, Gallo-Borrero CM, Santos-Areas D, Prince-Martínez IA, Díaz-Casañas E, López-Herce Cid J. Exogenous surfactant and alveolar recruitment in the treatment of acute respiratory distress syndrome. Clin Respir J. 2016;11(6):1032–1039. doi: 10.1111/crj.12462
4. Lewis JF, Veldhuizen R. The role of exogenous surfactant in the treatment of acute lung injury. Annu Rev Physiol. 2003;65:613–642. doi: 10.1146/annurev.physiol.65.092101.142434
5. Emeriaud G, López-Fernández YM, Iyer NP, Bembea MM, Agulnik A, Barbaro RP, et al. Executive summary of the second international guidelines for the diagnosis and management of pediatric acute respiratory distress syndrome (PALICC-2). Pediatr Crit Care Med. 2023;24(2):143–168. doi: 10.1097/PCC.0000000000003147
6. De Luca D, Cogo P, Kneyber MC, Biban P, Semple MG, Perez-Gil J, et al. Surfactant therapies for pediatric and neonatal ARDS: ESPNIC expert consensus opinion for future research steps. Crit Care. 2021;25:75. doi: 10.1186/s13054-021-03489-6
7. Šapina M, Olujic B, Nađ T, Vinkovic H, Dupan ZK, Bartulovic I, et al. Bronchoscopic treatment of pediatric atelectasis: a modified segmental insufflation–surfactant instillation technique. Pediatr Pulmonol. 2024;59(3):625–631. doi: 10.1002/ppul.26792
8. Stafler P, Zeitlin Y, Dotan M, Shostak E. Bronchoscopic lung insufflation and surfactant instillation for post-cardiac surgery atelectasis in a neonate. Pediatr Interv Pulmonol. 2025;2(1):15–17.
9. Puntorieri V, Qua Hiansen J, McCaig LA, Yao LJ, Veldhuizen RAW, Lewis JF. The effects of exogenous surfactant administration on ventilation-induced inflammation. BMC Pulm Med. 2013;13:55. doi: 10.1186/1471-2466-13-67
10. Schousboe P, Uslu B, Schousboe A, Nebrich L, Wiese L, Verder H, et al. Lung surfactant deficiency in severe respiratory failure: a potential biomarker for clinical assessment. Diagnostics. 2025;15:847. doi: 10.3390/diagnostics15070847
11. Cai J, Su Z, Zhou Y, Shi Z, Xu Z, Liu J, et al. Beneficial effect of exogenous surfactant in infants suffering acute respiratory distress syndrome after cardiac surgery. Eur J Cardiothorac Surg. 2011;40(3):557–562. doi: 10.1016/j.ejcts.2011.01.008
12. Guo R, Chen Y, Hu X, Qi Z, Guo J, Li Y et al. Phenylalanyl-tRNA synthetase deficiency caused by biallelic variants in the FARSA gene and literature review. BMC Med Genomics. 2023;16:155. doi: 10.1186/s12920-023-01662-0
13. Kim SY, Ko S, Kang H, Kim MJ, Moon J, Lim BC, et al. Fatal systemic disorder caused by biallelic variants in FARSA. Orphanet J Rare Dis. 2022;17:79. doi: 10.1186/s13023-022-02457-9
14. Schuch LA, Forstner M, Rapp CK, Li Y, Smith DEC, Mendes MI, et al. FARS1-related disorders caused by biallelic mutations: look beyond the lungs! Clin Genet. 2021;99(4):552–563. doi: 10.1111/cge.13943
15. Lomuscio S, Cocciadiferro D, Petrizzelli F, Liorni N, Mazza T, Allegorico A et al. Two novel biallelic variants in the FARSA gene: the first Italian case. Genes. 2024;15:412. doi: 10.3390/genes15121573
16. Charbit-Henrion F, Goguyer-Deschaumes R, Borensztajn K, Mirande M, Berthelet J, Rodrigues-Lima F, et al. Systemic inflammatory syndrome in children with FARSA deficiency. Clin Genet. 2022;102(3):211–219. doi: 10.1111/cge.14120