Bronchoscopic Lung Insufflation and Surfactant Instillation for Post-Cardiac Surgery Atelectasis in a Neonate
Main Article Content
Abstract
Introduction: Persistent atelectasis in neonates can result in impaired gas exchange and prolonged morbidity when conservative measures fail. Bronchoscopic insufflation with surfactant instillation has recently been described as a promising therapeutic option.
Methods: We report the case of a neonate with persistent and treatment unresponsive atelectasis following arterial switch operation. The lung insufflation technique described by Šapina et al. was adapted by using a Neopuff manometer connected between the oxygen wall outlet and the bronchoscope working channel. Under light general anaesthesia with midazolam and propofol, a pediatric flexible bronchoscope was used to perform lavage, segmental insufflation, and instillation of surfactant.
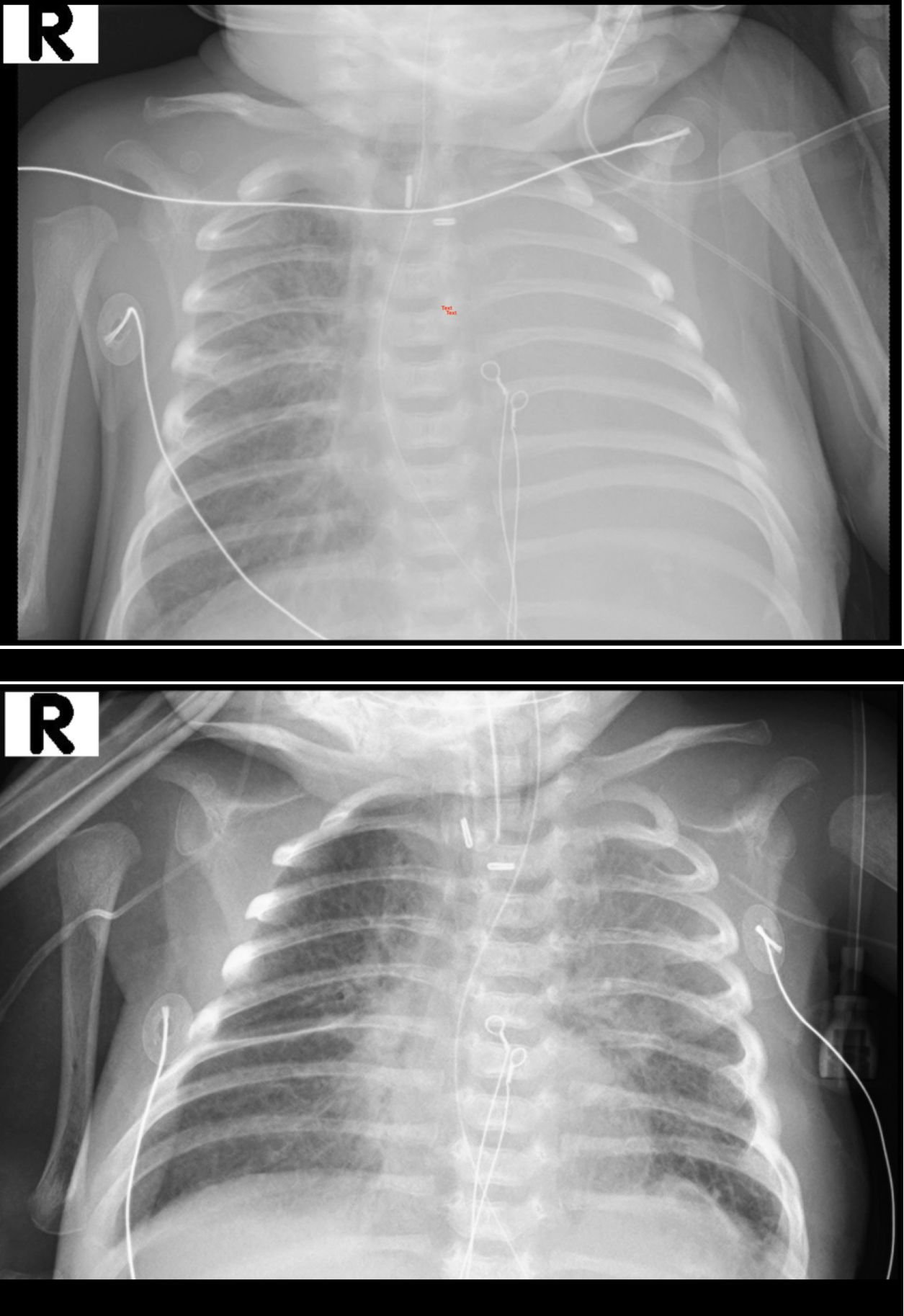
Results: After three insufflation cycles to 30 cm H2O and surfactant administration in two aliquots, elective intubation was maintained for 24 hours to preserve lung recruitment. Post-procedure, the left lung was re-aerated with no evidence of pneumothorax.
Conclusion: This case demonstrates the feasibility and safety of bronchoscopic pressure-controlled insufflation combined with surfactant instillation in a neonate post-cardiac surgery, supporting its utility as described in recent literature.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Share
References
1. Griese M, Wilnhammer C, Jansen S, and Rinker C. Cardiopulmonary bypass reduces pulmonary surfactant activity in infants. J Thorac Cardiovasc Surg. 1999;118:237–244. doi: 10.1016/S0022-5223(99)70213-8
2. Camassuti PAS, Johnston C, de Carvalho WB, Luglio M, de Araujo OR, and Morrow B. Structured respiratory physiotherapy protocol for resolution of atelectasis in pediatric intensive care. Clinics (Sao Paulo). 2024;79:100494. doi: 10.1016/j.clinsp.2024.100494
3. Gipsman AI, Bhandari A, and Bhandari V. Use of mucolytics and inhaled antibiotics in the NICU. J Perinatol. 2025;45:5–12. doi: 10.1038/s41372-024-02178-w
4. Cai J, Su Z, Zhou Y, Shi Z, Xu Z, Liu J, Xu Z, and Yang Y. Beneficial effect of exogenous surfactant in infants suffering acute respiratory distress syndrome after cardiac surgery. Eur J Cardiothorac Surg. 2011;40:557–562. doi: 10.1016/j.ejcts.2011.01.008
5. Krause MF, von Bismarck P, Oppermann HC, and Ankermann T. Bronchoscopic surfactant administration in pediatric patients with persistent lobar atelectasis. Respiration. 2008;75:100–104. doi: 10.1159/000088713
6. Moslehi MA. Bronchoscopic surfactant administration in premature neonate with persistent lobar atelectasis: the new concept. J Matern Fetal Neonatal Med. 2021;34:3277–3279. doi: 10.1080/14767058.2019.1680628
7. Sapina M, Olujic B, Nad T, Vinkovic H, Dupan ZK, Bartulovic I, Milas K, Kos M, Divkovic D, Zubcic Z, and Eric I. Bronchoscopic treatment of pediatric atelectasis: A modified segmental insufflation-surfactant instillation technique. Pediatr Pulmonol. 2024;59:625–631. doi: 10.1002/ppul.26792
8. Vedrenne-Cloquet M, Khirani S, Khemani R, Lesage F, Oualha M, Renolleau S, Chiumello D, Demoule A, and Fauroux B. Pleural and transpulmonary pressures to tailor protective ventilation in children. Thorax. 2023;78:97–105. doi: 10.1136/thorax-2021-218538