Bronchoscopic Lung Insufflation and Surfactant Instillation for Post-Cardiac Surgery Atelectasis in a Neonate
Abstract
Background: Persistent atelectasis in neonates can result in impaired gas exchange and prolonged morbidity when conservative measures fail. Bronchoscopic insufflation with surfactant instillation has recently been described as a promising therapeutic option.
Methods: We report the case of a neonate with persistent and treatment unresponsive atelectasis following arterial switch operation. The lung insufflation technique described by Šapina et al. was adapted by using a Neopuff manometer connected between the oxygen wall outlet and the bronchoscope working channel. Under light general anaesthesia with midazolam and propofol, a pediatric flexible bronchoscope was used to perform lavage, segmental insufflation, and instillation of surfactant.
Results: After three insufflation cycles to 30 cm H2O and surfactant administration in two aliquots, elective intubation was maintained for 24 hours to preserve lung recruitment. Post-procedure, the left lung was re-aerated with no evidence of pneumothorax.
Conclusion: This case demonstrates the feasibility and safety of bronchoscopic pressure-controlled insufflation combined with surfactant instillation in a neonate post-cardiac surgery, supporting its utility as described in recent literature.
Video
Introduction
Atelectasis is a frequent clinical challenge in neonates following cardiac surgery requiring cardiopulmonary bypass, where impaired mucociliary clearance, surfactant dysfunction and ventilator-induced lung injury contribute to alveolar collapapse (1).
Standard medical therapy including physiotherapy, mucolytics, bronchodilators and antibiotics is first-line, but often insufficient in severe or persistent cases (2, 3). Exogenous surfactant has been shown to restore alveolar stability, improve compliance, and facilitate re-expansion (4-6).
When conservative measures fail, bronchoscopic intervention may be warranted, though this carries added hazard in high-risk infants due to potential hemodynamic compromise. Careful patient selection and hemodynamic monitoring are therefore essential. Recently, Šapina et al. described a modified bronchoscopic technique that combines pressure-controlled segmental insufflation with surfactant instillation, achieving rapid and sustained lung re-expansion in young children (7). This evolving approach may provide a minimally invasive therapeutic option in otherwise refractory cases.
We present a video case that demonstrates the application of this technique in a neonate who developed persistent left-sided atelectasis following complex cardiac surgery, highlighting technical considerations and clinical outcome.
Case Description
A female neonate was born with transposition of the great arteries and had to undergo arterial switch surgery, combined with closure of atrial and ventricular septal defects on day two of life. Her recovery was complicated by pleural effusions, intermittent bilateral alveolar infiltrates and left sided diaphragmatic palsy, detected on post-operative day (POD) 15. On POD 25, she underwent left sided plication of her diaphragm. She was kept nil by mouth for 10 days due to chylothorax, and was treated with furosemide, spironolactone and hydrochlorothiazide for cardiac support, as well as oxycodone and diazepam for sedation withdrawal.
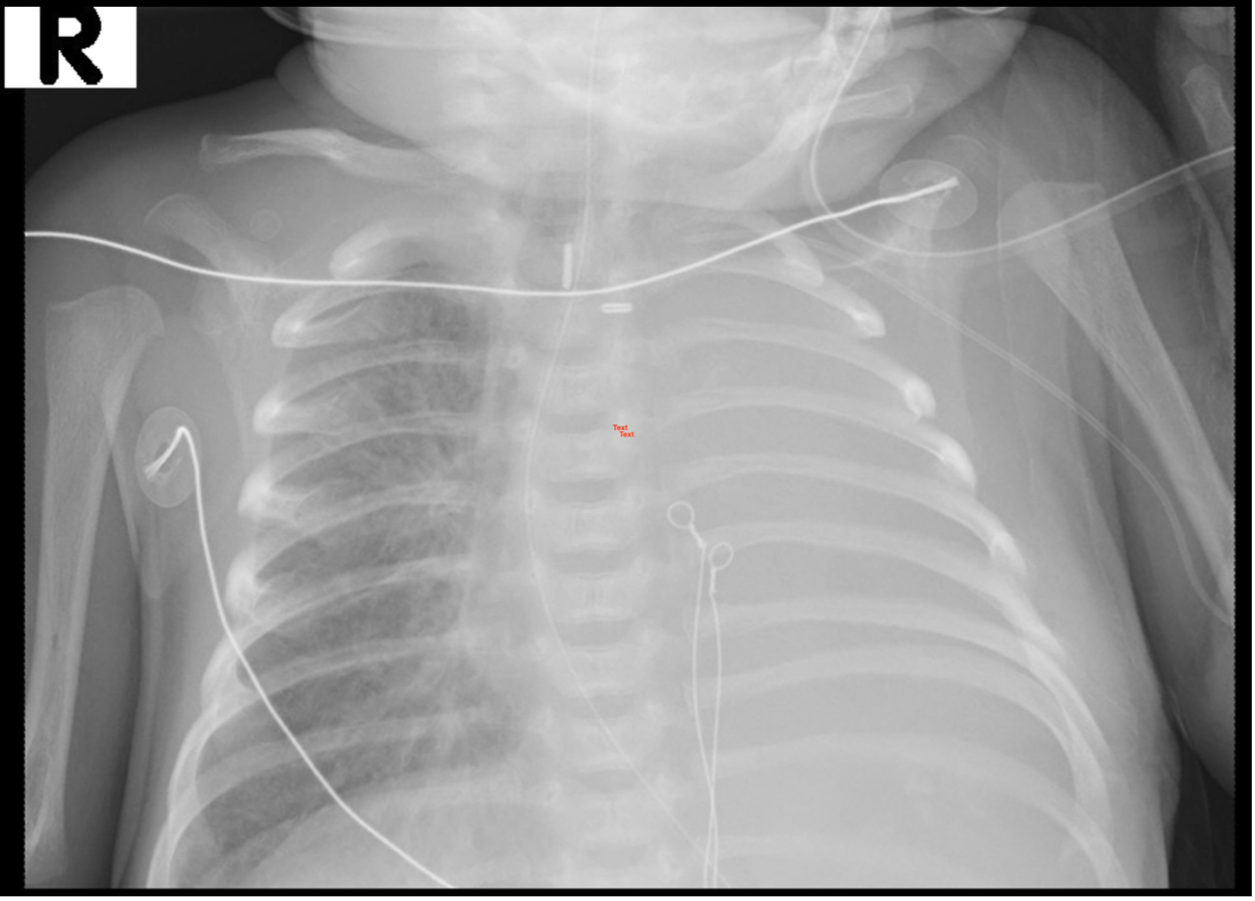
On POD 28, she developed dense collapse/ consolidation of her left lung (figure 1). This was unresponsive to three times daily chest physiotherapy, aided by inhaled hypertonic saline and intra-pulmonary percussion. She was supported with non-invasive ventilation using high flow nasal cannula and nasal bilevel positive airway pressure (BiPAP), prone positioning and antibiotic therapy. On POD 32, it was decided to proceed with bronchosocpy, surfactant instillation and lung insufflation, according to the technique published by Šapina et al., using minor modifications.
Procedure
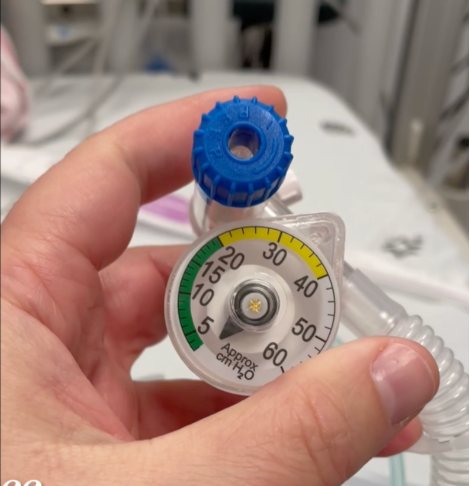
Setup: A disposable Neopuff manometer from a T-Piece Resuscitator System (Fisher & Paykel Healthcare, Auckland, New Zealand, figure 2) was connected to the oxygen wall outlet on one side and to the bronchoscope working channel on the other side. This allowed simultaneous oxygen delivery and continuous monitoring of insufflation pressure.
Sedation and airway access: The neonate was maintained on spontaneous ventilation under light general anaesthesia using midazolam and propofol. A 2.8 mm pediatric flexible bronchoscope (BF-XP60, Olympus, Tokyo, Japan) was introduced via the nasal route.
Bronchoalveolar lavage: Inspection for airway abnormalities was undertaken and diagnostic BAL performed in the left lung.
Segmental insufflation: The bronchoscope was advanced into a near-wedged position in the distal left main bronchus, avoiding complete occlusion to minimize risk of complications in this fragile infant. Pressure-controlled insufflation was performed, reaching 30 cm H2O for 30 seconds (figure 3).
Surfactant instillation: The standard endotracheal tube (ETT) dose of poractant alfa (Curosurf, 200 mg/kg) was halved. A dose of 100 mg/kg was administered to the left lung, divided equally as 50 mg/kg to the left upper lobe and 50 mg/kg to the left lower lobe (7).
Repetition: Two further cycles of insufflation were carried out with the same scope position, pressure and duration parameters.
Post-procedure management: Elective endotracheal intubation was undertaken for 24 hours to maximize chances of sustained lung recruitment and patency.
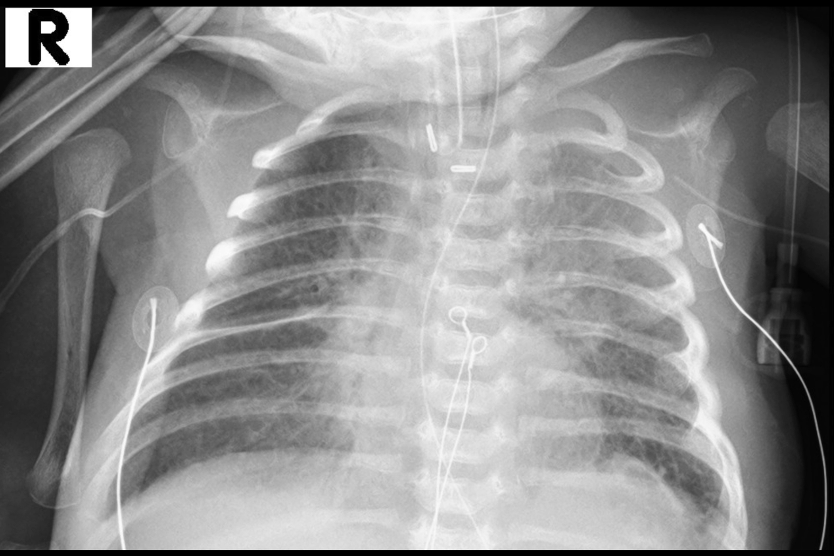
Outcome: Post-procedure imaging confirmed complete aeration of the left lung with no evidence of pneumothorax (figure 4). The neonate was extubated the following day and remained clinically stable. The post-extubation chest x-ray, as well as serial x-rays during the subsequent two weeks demonstrated no recurrence of atelectasis in the left lung.

Conclusion
This case illustrates the successful application of bronchoscopic pressure-controlled insufflation combined with surfactant instillation for persistent atelectasis in a neonate post-cardiac surgery. The technique, adapted from Šapina et al., was safe and effective, with rapid restoration of lung volume and no complications. Unlike manual “bolus” air insufflation or global recruitment maneuvers, a predefined pressure ceiling with real-time bronchoscopic visualization allows titrated, segment-targeted re-expansion while limiting peak and transpulmonary pressure swings that risk volutrauma/barotrauma and hemodynamic compromise in fragile post-operative infants (8). This reinforces the growing evidence for the role of bronchoscopic insufflation, in addition to the more established surfactant instillation as an additional therapeutic option for persistent atelectasis. That said, comparative evidence remains limited; our case is hypothesis-generating and cannot establish superiority.
Prospective studies - ideally with physiologic monitoring (e.g., lung ultrasound), standardized pressure caps/dosing schemas, and predefined hemodynamic criteria—are warranted to test whether segment-targeted, pressure-controlled insufflation with surfactant outperforms conventional bronchoscopic lavage/suction or global recruitment in time to re-expansion, need for re-intervention, and safety.
Conflict of interest
None to declare.
Data availability statement
There is no original data beyond those displayed in the submission.
Author contributions
PS: Conceived and planned the intervention, performed the bronchoscopic procedure, collected clinical data, and wrote the first draft of the manuscript and video narrative.
YZ: Provided anesthesia management during the procedure, contributed to peri-procedural care, and critically reviewed the manuscript.
MD: Contributed to peri-procedural care and critically reviewed the manuscript.
ES: Responsible for patient care in the intensive care unit, coordinated multidisciplinary management, and reviewed and edited the manuscript for intellectual content.
All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Ethical statement
The procedure was performed as part of routine clinical care. Institutional policy waived the need for specific ethics committee approval or written informed consent for this case report.
References
1. Griese M, Wilnhammer C, Jansen S, Rinker C. Cardiopulmonary bypass reduces pulmonary surfactant activity in infants. J Thorac Cardiovasc Surg. 1999 Aug;118(2):237–44. doi: 10.1016/S0022-5223(99)70213-8
2. Camassuti PAS, Johnston C, de Carvalho WB, Luglio M, de Araujo OR, Morrow B. Structured respiratory physiotherapy protocol for resolution of atelectasis in pediatric intensive care. Clinics (Sao Paulo). 2024 Nov;79:100494. doi: 10.1016/j.clinsp.2024.100494
3. Gipsman AI, Bhandari A, Bhandari V. Use of mucolytics and inhaled antibiotics in the NICU. J Perinatol. 2025 Jan;45(1):5–12. doi: 10.1038/s41372-024-02178-w
4. Cai J, Su Z, Zhou Y, Shi Z, Xu Z, Liu J, Xu Z, Yang Y. Beneficial effect of exogenous surfactant in infants suffering acute respiratory distress syndrome after cardiac surgery. Eur J Cardiothorac Surg. 2011 Sep;40(3):557–62. doi: 10.1016/j.ejcts.2011.01.008
5. Krause MF, von Bismarck P, Oppermann HC, Ankermann T. Bronchoscopic surfactant administration in pediatric patients with persistent lobar atelectasis. Respiration. 2008 Sep;75(1):100–4. doi: 10.1159/000088713
6. Moslehi MA. Bronchoscopic surfactant administration in premature neonate with persistent lobar atelectasis: the new concept. J Matern Fetal Neonatal Med. 2021 Oct;34(19):3277–79. doi: 10.1080/14767058.2019.1680628
7. Sapina M, Olujic B, Nad T, Vinkovic H, Dupan ZK, Bartulovic I, Milas K, Kos M, Divkovic D, Zubcic Z et al. Bronchoscopic treatment of pediatric atelectasis: A modified segmental insufflation-surfactant instillation technique. Pediatr Pulmonol. 2024 Mar;59(3):625–31. doi: 10.1002/ppul.26792
Vedrenne-Cloquet M, Khirani S, Khemani R, Lesage F, Oualha M, Renolleau S, Chiumello D, Demoule A, Fauroux B. Pleural and transpulmonary pressures to tailor protective ventilation in children. Thorax. 2023 Jan;78(1):97–105. doi: 10.1136/thorax-2021-218538
Submitted: August 24, 2025
Accepted: September 4, 2025
Published: September 6, 2025
© 2025 Stafler et al. This open-access article is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0).